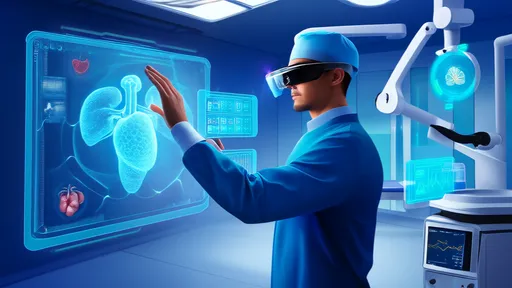
The operating room hums with a familiar tension, but something is different. A surgeon, hundreds of miles from the patient on the table, is not peering over a junior colleague’s shoulder via a shaky video feed. Instead, they are virtually present, their digital avatar standing beside the primary surgeon, who is wearing a sleek headset. With a gesture, the remote expert draws a precise, glowing incision line directly onto the patient’s anatomy, visible only through the lens of extended reality. This is not a scene from science fiction; it is the rapidly evolving present of remote surgical guidance, powered by Extended Reality (XR).
Extended Reality, an umbrella term encompassing Virtual Reality (VR), Augmented Reality (AR), and Mixed Reality (MR), is dismantling the traditional barriers of geographical distance in medicine. While telemedicine has long offered basic consultation through video calls, XR injects a profound layer of immersion and spatial understanding. It allows for a collaborative environment where medical professionals can share not just data, but a simulated physical space. The implications for surgical training, complex procedure planning, and real-time intraoperative guidance are nothing short of revolutionary, promising to democratize access to world-class surgical expertise.
The technological foundation of this revolution rests on a convergence of advanced hardware and sophisticated software. High-fidelity headsets, like the Microsoft HoloLens or Magic Leap, provide the visual gateway, overlaying digital information onto the real world or creating entirely virtual operating theaters. These are complemented by haptic feedback devices that simulate the sense of touch, allowing a remote mentor to feel the resistance of tissue or the pulsation of a vessel through robotic intermediaries. Crucially, ultra-low latency 5G networks form the circulatory system of this setup, ensuring that the data stream—a constant flow of high-definition video, 3D anatomical models, and sensor data—is transmitted without perceptible delay. A fraction of a second lag could be the difference between a successful intervention and a catastrophic error.
In practice, the application of XR begins long before the first incision is made. Surgical teams are using VR to rehearse complex procedures on patient-specific 3D anatomical models generated from CT or MRI scans. A surgeon can walk through the entire operation, identifying potential challenges and planning the optimal approach. This digital rehearsal space eliminates risk and builds muscle memory. When the day of the surgery arrives, AR takes center stage. The primary surgeon, wearing an AR headset, can see critical information—such as the location of major blood vessels or tumors—projected directly onto the patient’s body. This X-ray vision enhances precision and reduces the cognitive load of constantly shifting focus between the patient and external monitors.
The most transformative aspect, however, is live, remote collaboration. Imagine a challenging rural hospital where a general surgeon must perform a specialized procedure. Using an XR platform, they can connect with a leading specialist in a metropolitan center. The remote expert sees everything the local surgeon sees through a calibrated feed. They can then annotate the surgical field with arrows, lines, and text that appear as holograms in the local surgeon’s field of view. The remote mentor can literally point to the exact spot that requires attention or manipulate a 3D model of the anatomy to explain a complex step. This guided experience is far more intuitive and effective than audio instructions alone, closely approximating the experience of having the expert physically in the room.
Despite the immense promise, the path to widespread adoption is not without significant hurdles. The foremost concern is that of data security and patient privacy. Transmitting real-time surgical feeds and sensitive patient data over networks requires impregnable encryption and robust cybersecurity protocols to prevent devastating breaches. Furthermore, the technology itself must achieve a level of reliability that meets the unforgiving standards of healthcare. Glitches, software crashes, or network dropouts are simply not acceptable in a life-or-death environment. The high cost of cutting-edge XR equipment and the need for specialized IT support also present substantial financial barriers for many healthcare institutions, potentially exacerbating existing disparities in healthcare access.
Looking ahead, the trajectory of XR in remote surgery points toward even greater integration and automation. The next frontier involves the fusion of XR with artificial intelligence and robotics. AI algorithms could analyze the surgical video feed in real-time, offering predictive alerts about potential complications or suggesting the next steps in a procedure. This AI co-pilot would augment the abilities of both the local and remote surgeon. Furthermore, the annotations made by a remote expert could be translated into commands for robotic surgical systems, allowing for a form of telepresence surgery where the expert’s guidance directly influences the movements of robotic arms. This creates a powerful synergy between human expertise and machine precision.
In conclusion, Extended Reality is fundamentally reshaping the landscape of surgical care and mentorship. It is transforming remote guidance from a passive, advisory role into an active, immersive partnership. By enabling experts to be virtually hands-on from any location in the world, XR is breaking down the walls of the operating room and paving the way for a future where high-quality surgical expertise is a universally accessible resource, not a privilege of geography. The journey involves overcoming substantial technical and ethical challenges, but the potential to save lives, standardize care, and elevate the skills of surgeons everywhere makes it one of the most compelling chapters in the ongoing story of medical innovation.

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025
By /Aug 26, 2025

By /Aug 26, 2025
By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025

By /Aug 26, 2025
By /Aug 26, 2025

By /Aug 26, 2025
By /Aug 26, 2025
By /Aug 26, 2025